Reducing Your Risk for Lymphedema After Breast Cancer Treatment
Lymphedema is a buildup of fluid that causes swelling. It can happen after breast surgery or radiation to your chest or armpit to treat breast cancer. Fluid can build up and cause swelling in the treated areas. This can happen at any time. It can happen even many years after treatment. You need to know what breast cancer-related lymphedema is and what to watch for.
Your healthcare team will check you for breast cancer-related lymphedema. Before surgery or radiation, your arms may be measured and the sizes recorded. Then, after treatment, your arms can be remeasured at each visit. This is done so that swelling can be found and treated right away. Treating lymphedema soon can help keep it from getting worse.
Your healthcare provider will check your height and weight before treatment. Your weight will be checked at every follow-up visit. Gaining weight can put you at a higher risk for lymphedema.
There's no sure way to know who will get breast cancer-related lymphedema or how to prevent it. And once the swelling starts, there's no sure way to cure it. You are at risk for lymphedema for the rest of your life. Because of this, it's important to know what it is, what you can do to help reduce your risk, and what you should watch for.
You can ask your healthcare provider for a referral to a certified lymphedema therapist. This is a provider who focuses on lymphedema teaching and management.
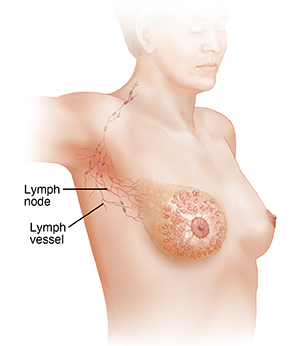
How does the lymphatic (lymph) system work?
The lymphatic system is part of your immune system. It’s a network of tiny vessels and small, bean-shaped organs called lymph nodes that are found along the vessels. Your lymphatic system goes throughout your whole body, like blood vessels. But instead of carrying blood, it carries lymph. Lymph is a clear fluid that has white blood cells. Your lymphatic system helps your body maintain fluid balance and filters lymph to help fight infection.
How does breast cancer-related lymphedema happen?
Lymphedema can happen after breast cancer when surgery is done to remove lymph nodes and vessels from under the arm. Or it can happen when the underarm area is treated with radiation therapy. These treatments damage the underarm (axillary) lymph nodes and the nearby lymph vessels. This disrupts the normal flow of lymph in the hand, arm, underarm, chest, neck, and breast. So instead of lymph flowing through your lymphatic system and back to your blood vessels like it should, the fluid collects in your skin and tissues. This causes swelling. The changes in the flow of lymph also keep the lymph from being filtered the way it should. This can increase your risk for infections. It can interfere with wound healing in the affected areas.
What are the symptoms of breast cancer-related lymphedema?
The main symptom of lymphedema after breast cancer treatment is swelling of the hand or arm on the treated side of your body. Your chest, underarm, and neck can swell, too. It usually starts slowly. The affected arm may be only slightly bigger than the other arm. You may be able to see a difference when comparing both sides of your body. You may notice that your jewelry seems tighter. The amount of swelling can vary at first. But over time, if not treated, it can become severe. The affected arm may be several inches bigger than the other arm.
It’s important to know that mild lymphedema is normal for a few days after breast surgery. This usually lasts a short time. The more serious type of lymphedema starts later, often a few months to years after surgery or radiation. This can become long-lasting (chronic) lymphedema that doesn’t go away.
Other symptoms of breast cancer-related lymphedema that you can watch for are:
-
Feeling of fullness, heaviness, or tightness in your arm, chest, or armpit
-
Bra, clothing, or jewelry doesn't fit like it usually does
-
Aching or new pain in your arm
-
Trouble bending or moving a joint, such as the fingers, wrist, elbow, or shoulder
-
Swelling or tightness in your hand
-
Thickening of or changes in your skin
-
Weakness in your arm
If you notice any of these changes on the treated side of your body, see your healthcare provider right away. Treatment may be needed. For instance, swelling could be a sign of lymphedema, but swelling along with redness or warmth could be a sign of infection. In either case, treatment needs to be started right away.
What affects my risk for breast cancer-related lymphedema?
Any person who’s had surgery or radiation to the breast, chest, and armpit as breast cancer treatment has some risk for lymphedema. And it can occur months or years after treatment. But some factors are linked to a higher risk for breast cancer-related lymphedema, such as:
-
The number of lymph nodes removed or damaged increases risk. The more nodes and nearby lymph vessels affected, the greater the risk.
-
Radiation therapy to the breast, chest, and armpit damages the lymph system in these areas and increases risk. The risk may be even higher if you had both surgery and radiation.
-
Infection or inflammation in the affected areas is linked to the start of lymphedema.
-
Being obese (BMI of 30 or higher), being overweight (BMI 25 to 29), and gaining weight after treatment are all linked to a higher chance of lymphedema.
-
Not enough physical activity and not using your affected arm may raise your risk for lymphedema.
How can I reduce my risk for breast cancer-related lymphedema?
There’s no sure way to know who will get lymphedema or how to prevent it. Not all experts agree on what might help reduce risk, but here are some things you can do:
-
Get follow-up care. See your healthcare provider on a regular basis for checkups. Ask about seeing a certified lymphedema specialist to learn more about breast cancer-related lymphedema and how you can try to prevent it.
-
Watch for signs of lymphedema. Take note of how your hand, arm, and chest normally feel and look after treatment. Compare the sides of your body. Look for changes. If you notice any changes, let your provider know right away. The sooner the swelling is treated, the better the chances of reducing it and keeping it from getting worse.
-
Prevent infection. There are some simple things you can do to help protect your at-risk arm from infection. For instance, wash, treat, and cover any skin wounds, even the smallest cut, scratch, or burn. Check your skin regularly. Don’t pick at or bite your cuticles. Use a cuticle stick to push them back. And use sunscreen and insect repellent to protect your skin when you’re outside. Wear gloves when you garden, use a harsh chemical, or handle garbage. Be careful to prevent sunburns and burns from cooking. Keep your skin clean, and use lotion to keep it soft. Ask your provider for more tips. It’s important to prevent infections and maybe even more important to watch for the first sign of infection and get treatment right away.
-
Keep moving. Do your arm exercises. Don’t avoid using your affected arm. After you heal, use it like you normally would. It’s also good to exercise your whole body. But first talk with your healthcare team about the type of exercise that’s best for you. You can ask to see a lymphedema specialist to learn safe exercises and what your goals and limits might be.
-
Watch your weight. Being overweight or gaining weight after treatment can put you at a higher risk for lymphedema. Talk with your healthcare team about your weight and what’s healthy for you. Ask them for advice on how to get to that weight and stay there.
Talk with your healthcare team about your risk for lymphedema and what you can do to help keep it from starting. Here are some other things you may want to ask your provider about:
-
Is it OK to have your blood pressure taken in your at-risk arm? You may be advised by your healthcare provider to not have your blood pressure taken in your at-risk arm. Check with your healthcare provider.
-
Is it OK to have blood drawn or an IV (intravenous) line put in your at-risk arm? You may be advised by your healthcare provider to not have your blood drawn or put an IV in your at-risk arm. Check with your healthcare provider.
-
What’s the best way to care for and watch your skin? What’s normal for you now? (If you had surgery or radiation, the treated parts of your body may look and feel different.)
-
Should you take arm measurements? If so, how do you do it and how often should you measure?
-
Are there any types of clothes you need to wear or not wear?
-
Do you need to take any extra care when you travel?
You are at risk for lymphedema for the rest of your life, so talk with your healthcare team and try to make their advice part of your regular habits.
When should I call my healthcare provider?
Call your healthcare provider right away if you have:
-
Fever of 100.4ºF (38ºC) or higher, or as directed by your healthcare provider
-
Any of these changes in the at-risk arm, armpit, chest, or neck:
-
Signs of infection such as red blotches, warmth, or pain
-
Sudden new swelling
-
New heaviness or weakness
-
New pain
-
Cracking or peeling skin
Ask your healthcare provider what signs to watch for and when to call. Know how to get help after office hours and on weekends and holidays.