When Your Child Has Intussusception
The bowel (intestine) is a very long tube. It's coiled up inside the belly (abdomen). Intussusception occurs when a part of the bowel slides inside another part. This happens in the same way that parts of a telescope slide inside each other. The bowel can slide back out by itself. Or it can get stuck. Blood flow to part of the bowel could then be blocked. This can cause severe harm if not treated. Intussusception can happen anywhere in the bowel. It’s most common near where the large intestine and small intestine meet. Most cases of intussusception occur by age 3.
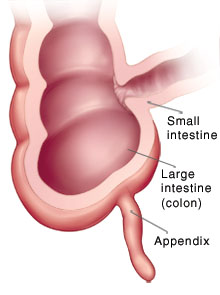 |
| Intussusception can happen in any part of either intestine. But, it often happens where the small intestine and large intestine meet. |
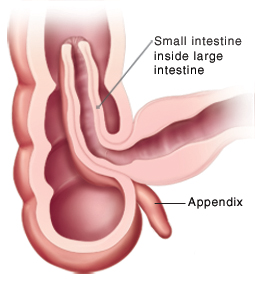 |
| Intussusception happens when part of one intestine slips inside the other intestine. |
What are the symptoms of intussusception?
Intussusception is very painful. Symptoms often occur suddenly. They may continue if the bowel gets stuck inside the other part. Or symptoms may go away and come back if part of the bowel keeps sliding in and out of the other part. Symptoms may include:
-
Severe abdominal pain (a baby may cry and not be soothed)
-
Abdominal pain that is sudden and gets worse, then goes away for 15 to 20 minutes, then comes back
-
Vomiting that may have green bile in it
-
Bloody stools with mucus in them, known as currant jelly stools
-
Abdominal swelling
-
Diarrhea
-
Signs of dehydration, such as less urine, dark urine, dry mouth, no tears when crying
-
Changed mental state or lethargy (excessive sleepiness) as symptoms get worse
How is intussusception diagnosed?
Your child’s healthcare provider will ask about your child’s symptoms and health history. They will give your child a physical exam. Your child may then have tests such as:
-
Abdominal X-ray. X-rays create images of the inside of the body.
-
CT scan. This test creates 3-D images of the inside of the abdomen.
-
MRI. Strong magnets and radio waves are used to form an image of the inside of the abdomen.
-
Abdominal ultrasound. Sound waves are used to create a moving image of the inside of the abdomen.
-
Fluid or air enema. Either a contrast liquid or air is inserted into the rectum through the anus. This makes the bowel show up very clearly when a special scan is done.
How is intussusception treated?
To treat the problem, a fluid or air enema may be done. The force of the fluid or air entering the bowel can straighten it. Most cases are treated this way. If this doesn't work, surgery must be done. During surgery, the slipped portion of bowel is straightened, then checked for damage. If part of the bowel has been damaged due to lack of blood flow, that part may need to be removed. The healthy ends of the bowel are then reattached.
What are the long-term concerns?
Most children do well after treatment. If part of the bowel must be removed, your child could have long-term digestive problems. But this is very rare. Your child’s healthcare provider will tell you more. Even after it’s treated, intussusception could happen again. You’ll need to watch for symptoms. As your child gets older, intussusception is less likely to happen.
When intussusception goes away and comes back
Intussusception is an emergency if a part of the bowel gets stuck. But the problem can come and go. This means that the bowel slides inside itself, then slides back into correct position. Tests can only see the problem when it is happening. If the bowel has returned to normal position at the time of the test, the healthcare provider can’t diagnose it at that time. If your child has symptoms again, they need to return to the provider or the emergency room.